 Read more
Read more

Track employee hours, manage benefit eligibility, and generate the reports you need to stay compliant with ACA requirements.
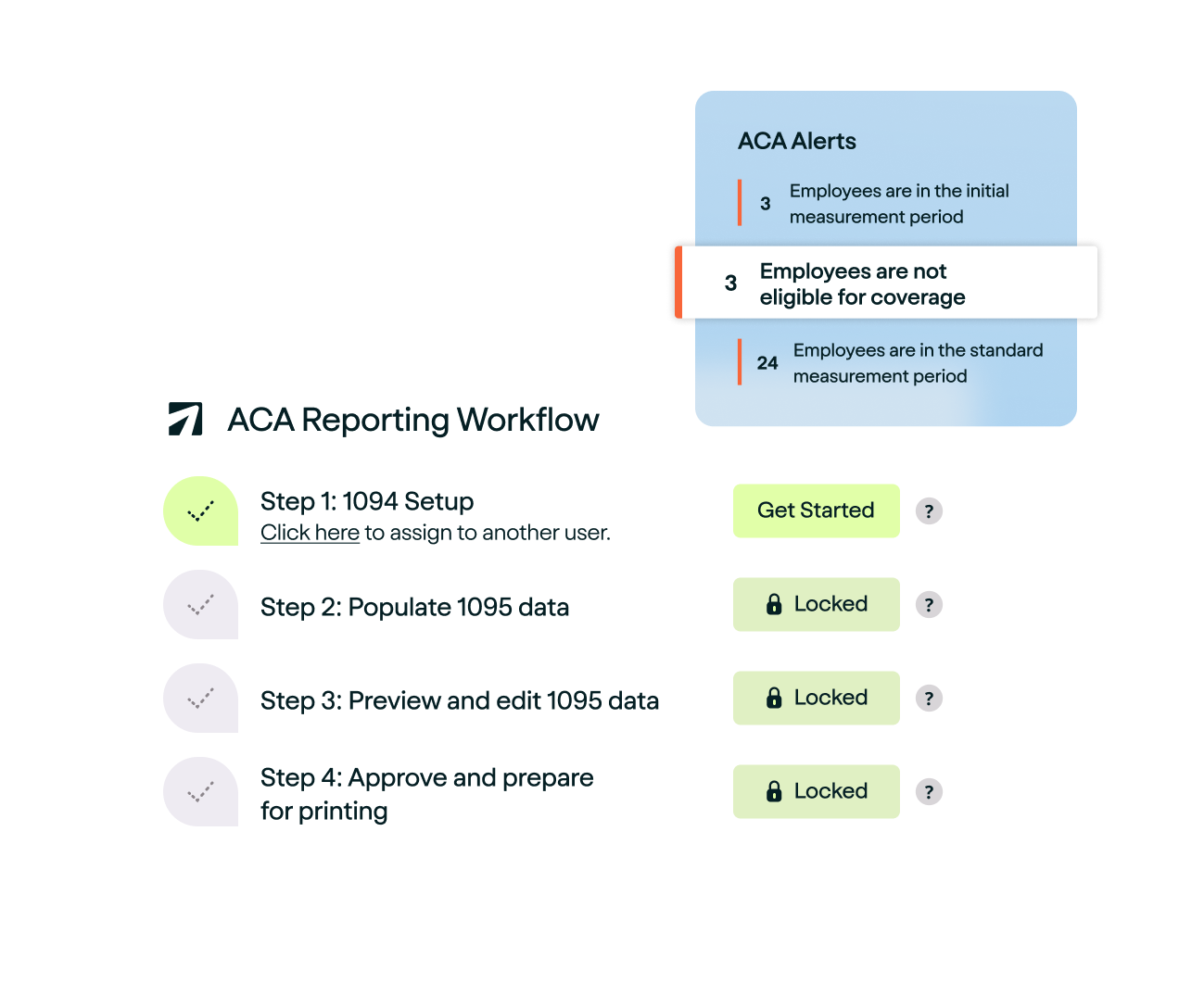









Whether tracking part-time employees or adapting to evolving regulations, APS helps you navigate ACA requirements.

Leverage our ACA reporting software’s built-in tools for eligibility tracking, form generation, and e-filing all in one seamless platform.
Quickly calculate full-time equivalents (FTEs) and determine Applicable Large Employer (ALE) status without manual calculations.
Generate, review, approve, and e-file your 1094-C and 1095-C forms with our streamlined ACA reporting services in a few clicks.
Track benefit plan eligibility and enrollment in real time with ACA enrollment software configured to meet your company’s needs.

ACA compliance is the process of an Applicable Large Employer (ALE) offering health insurance coverage to eligible employees in accordance with the Affordable Care Act. ALEs are employers with 50 or more full-time employees working at least 30 hours per week or their equivalents when adding together part-time hours.
ALEs are required to offer health insurance coverage that meets the ACA’s specifications to at least 95% of full-time employees or pay the penalty. Businesses with fewer than 50 employees are exempt from the employer mandate. However, if they choose to offer health insurance coverage to their full-time employees, it must meet the ACA’s specifications.
The ACA’s specifications for health insurance coverage require that a plan must offer minimum essential coverage (MEC). Examples of plans that count as qualifying health coverage include:
A health insurance plan must also provide minimum value, meaning the plan pays for at least 60% of covered benefits.
ALEs must report on the health insurance coverage they have offered each calendar year under the employer information reporting provision. This process consists of employers using Form 1094-C, Transmittal of Employer-Provided Health Insurance Offer and Coverage Information Returns, and Form 1095-C, Employer-Provided Health Insurance Offer and Coverage. Use these forms to report the following required information:
Applicable large employers must follow these guidelines as required by the Affordable Care Act to ensure they are ACA compliant.
Employers do need to report COBRA coverage for ACA compliance, depending on the situation. An employer does not need to report an offer of COBRA continuation coverage to a former employee due to termination of employment in Part II of Form 1095-C.
An employer does need to report an offer of COBRA continuation coverage to an active employee who loses eligibility for non-COBRA coverage due to a reduction in hours in Part II of Form 1095-C. An example of a loss of eligibility for non-COBRA coverage would be a change from full-time to part-time status, resulting in a loss of eligibility under the health plan.
Let’s say an employer sponsors a self-insured health plan, and an employee’s spouse and dependents have separately elected to receive COBRA continuation coverage. In this case, the employer may choose to report coverage of each non-employee spouse and dependent who separately elects COBRA continuation coverage on Form 1095-B or Form 1095-C.
An example of this would be if an employee divorced their spouse and the spouse separately elected to receive COBRA continuation coverage. The employer would report the employee’s enrollment in Part III of Form 1095-C and the months of the calendar year that the spouse had coverage.
A full-time employee who terminates employment during a calendar year and receives an offer of post-employment coverage is not reported as an offer of coverage in Part II of Form 1095-C. An example of this situation would be an employee’s retirement.
For more information on what codes to use, see the IRS’ Reporting Offers of COBRA Continuation Coverage and Post-Employment Coverage.
If your company is considered an Applicable Large Employer with 50 or more full-time equivalent employees, you need to worry about ACA compliance. Failure to offer a health insurance plan that provides minimum essential coverage (MEC) and minimum value will result in penalties assessed. These penalties include:
$2,700 per full-time employee minus the first 30 for failure to offer minimum essential coverage to at least 95% of full-time employees.
$4,600 divided by 12 for each full-time employee receiving subsidized coverage through an exchange for the month, for failure to provide coverage that is unaffordable or does not provide minimum value.
There are also penalties associated with the information reporting of ACA coverage:
These penalties can quickly add up. Therefore, it’s critical for companies that are subject to the employer mandate to have a plan in place that ensures continued compliance with the Affordable Care Act. Using compliance software like APS will automate these tasks and make Affordable Care Act compliance easier to manage.
Get started with pricing as low as $50 base fee/month + $6/employee per month. View Pricing
By clicking Get Started, you confirm your agreement with our Terms and Conditions.